SCHEDULE FREE CONSULTATION
Optimized Verification & Prior Authorization Services
At CareCloud MB, we simplify Verification & Prior Authorization Services to ensure timely, accurate processing. Our expert team navigates complex insurance requirements to minimize claim denials and delays, allowing healthcare providers to focus on patient care.
We streamline financial operations, improve revenue cycles, and eliminate inefficiencies, providing strategic guidance to enhance your practice’s growth and financial stability.
Schedule Free Consultation
Efficient Verification & Authorization
We use advanced tools and expertise to streamline your verification and prior authorization, ensuring faster, more accurate processing for smoother operations.
Boosted Revenue Collection
Our strategies reduce denials and delays, increasing collections by 5-10%. We streamline verification and authorization for faster approvals and higher first-submission success, boosting your practice’s revenue cycle.
Fast Authorization Processing
With cutting-edge technology, we quickly identify and resolve authorization issues, minimizing delays and maintaining a steady cash flow.

WHY CHOOSE US
How CareCloud MB Makes a Difference in the Authorization Process
- Help healthcare providers enhance the revenue cycle with the best Medical Billing services.
- Enhance revenue cycles with our expert verification and authorization services.
- Adopt advanced technology to prevent workflow disruptions.
- Leverage the best talent and strategies to optimize your practice’s financial health.
- Quickly identify and resolve issues causing delays or denials in authorization.
- Ensure compliance with industry regulations for higher approval rates.
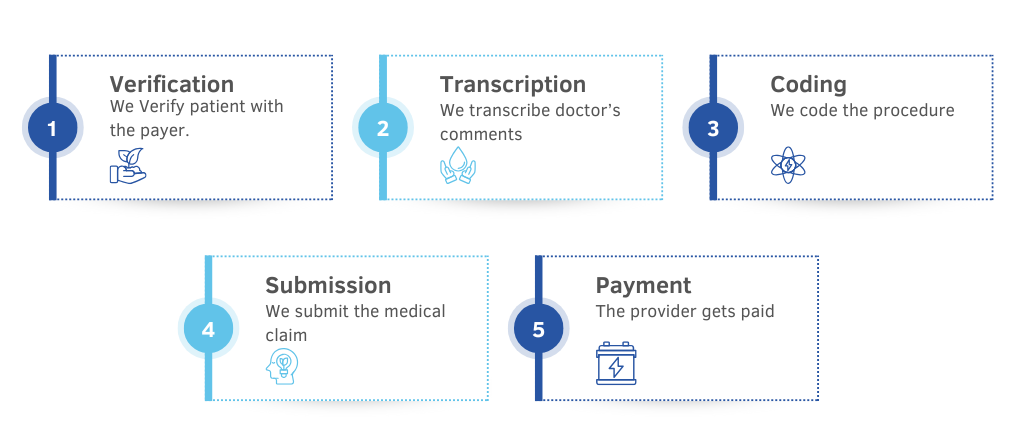
How Our Billing Process Works?
WHAT DO WE OFFER
Unlocking Growth Potential with Expert Verification & Prior Authorization Services
The verification and prior authorization process is often hindered by delays and errors, disrupting your practice’s cash flow and preventing you from reaching your goals. At CareCloud MB, we offer advanced solutions that eliminate these challenges, ensuring faster approvals, reducing denials, and accelerating revenue growth for your healthcare practice.
Detailed Analysis and Bill Reporting
- Reporting on RVU to calculate the value of medical services
- Clearing up hidden glitches for better revenue collection
- Clearing up hidden glitches for better revenue collection
- Providing detailed billing reports
Proper Service Level Agreements
- Dealing with payment posting for healthy cash flow
- Doing charge entry for service payments
- Reviewing denials with quick clear-ups
- Creating specialty-specific SLA reports
- Tracking accounts receivable aging
Revenue Leakage Fix
- Identifying and resolving errors
- Coding medical records
- Benchmarking the coding
- Auditing medical records

Best Billing Associates
- Modern technology for fast claim processing
- Medical billing with 24/7 physician support
- Ensuring correct patient billing
Maximizing Clean Billing Claims %
- Identifying trends and patterns in claims data
- Tracking all aspects of the claims process
- Using advanced data analysis tools
- Appealing on denied claims
- Keeping the provider in loop
Specialty Specific Specialization
- Staying updated on the latest changes in healthcare regulations
- Offering tailor-made solutions to small and medium practices
- Providing comprehensive services for improved bottom line
- Resolving RCM-related challenges for every specialty
- Supporting medical practitioners of all specialties

Exploring Growth Opportunities with Expert Verification & Prior Authorization Services
CareCloud MB Consultancy Features
Why Choose CareCloud MB for Verification & Prior Authorization Services
Authorization Insights
Gain valuable insights into key metrics like pending authorizations, approval rates, and denials per payer.
Track Authorizations
Monitor patient and insurance authorizations to measure approval times, identify trends, and ensure timely patient care.
Patient Follow-ups
Send reminder notices to patients for outstanding authorizations, reducing delays in treatment.
Automated Verification
Verify patient insurance benefits during check-in, ensuring all required authorizations are in place before treatment.
Performance Metrics
Track trends and get an overview of authorization statuses to improve approval rates.
Follow-up Process
Summarize pending and processed authorizations, with specialists following up to ensure approvals.
AI Workflow
AI detects and resolves authorization issues, ensuring faster approvals and fewer denials.
Smart Processing
Accurate coding and workflows ensure compliance and reduce errors in approval submissions.
Compliance Checks
AI algorithms suggest appropriate authorization levels to prevent fraud and ensure compliance.
GET FAIRLY PAID EVERY TIME
Elevate Your Practice with Expert Verification & Prior Authorization Services
Trusted Prior Authorization Services
Leading Authorization Practices
Revolutionizing Your Practice